Covered California Announces Launch of Population Health Investments in Conjunction With Its Quality Transformation Initiative
SACRAMENTO, Calif. — Covered California announced the launch of an innovative initiative that will reinvest millions of dollars collected from underperforming health plans back into its enrollees through programs designed to benefit their wellness.
Known as the Population Health Investments (PopHI) program, it will use funds that Covered California has recouped through its health-plan accountability program, the Quality Transformation Initiative. This initiative is aimed at improving health outcomes and reducing disparities for enrollees. It establishes direct financial incentives (up to 4 percent of premium) for contracted health insurance companies to meet specified quality benchmarks. The health outcome measures assessed include blood pressure and diabetes control, colorectal cancer screenings and childhood immunizations.
One PopHI program, which is known to enrollees as the Beyond Covered by Covered California Grocery Support Program, is designed to help enrollees with chronic health conditions and financial challenges access nutritious food to improve food security and health outcomes. The other PopHI program, the Child Savings Account Program, aims to improve well-child visits and childhood immunization rates for children under two while helping families invest in their child’s future.
Covered California’s third investment is aimed at leveraging the Equity and Practice Transformation infrastructure, developed by the Department of Health Care Services to accelerate population-health management capabilities in primary care practices serving both Covered California and Medi-Cal enrollees. The investments will fund subject-matter expert support, virtual learnings, peer engagement, advanced data integration and testing, as well as the development of a learning system to distill insights and models to primary care practices across the state.
For this program, over 45 practices will receive enhanced support through tailored enhancements to the Equity and Practice Transformation’s technical assistance structure.
“We are delighted to make these investments a reality,” said Dr. Monica Soni, Covered California’s chief medical officer and leader of the program’s implementation team. “This is about holding health plans accountable for high-quality care, while also reinvesting in the health and wellness of Californians.”
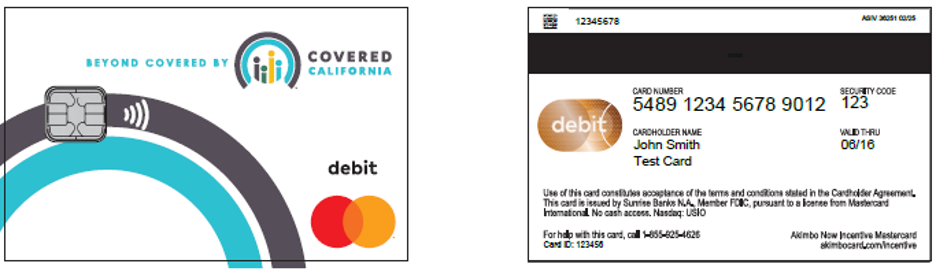
Covered California members with a household income up to 250 percent of the federal poverty level who have a chronic health issue and are experiencing food insecurity will be eligible for the Grocery Support Program, in which they receive a reloadable debit card to purchase food.
Funds will be based on household size reported at the time of enrollment and may only be used to purchase fresh food, packaged food, baby food and non-alcoholic drinks.
Figure 1: Grocery Support Program Debit Cards for Qualifying Members
Covered California enrollees with children under the age of two who are born in California and registered for a CalKIDS account can earn up to $1,000 for their child’s savings account, which can be used for future higher educational expenses under the Child Savings Account program. Payments are tied to the completion of well-child visits and receipt of vaccines according to clinical guidelines.
“We wanted to address the concerns raised by our members when choosing how to make the investments,” Covered California Executive Director Jessica Altman said. “Together, the programs aim to improve immediate health outcomes, but also foster long-term financial security, because our commitment is to reducing health disparities and enhancing the quality of life for all our members.”
These investments reflect Covered California’s commitment to evidence-based interventions developed in collaboration with consumer advocates, health insurance companies, the Department of Health Care Services, CalPERS, and an advisory council composed of key stakeholders and subject matter experts, including a current Covered California enrollee.
“California is pioneering a bold step in public health and child development with Beyond Covered,” said State Treasurer Fiona Ma, Chair of the ScholarShare Investment Board, which administers the CalKIDS Program. “In partnership with Covered California, CalKIDS is laying the foundation for a healthier, more equitable state for every child.”
FORWARD, a sponsoring entity for one of the programs, manages outreach, enrollment and member support, facilitating a streamlined process for participants to alleviate food insecurity and improve overall health outcomes. The Population Health Learning Center is the second program sponsoring entity, providing support and technical assistance for the primary care practices.
All of the programs will run through March 2026. The Grocery Support Program will then be evaluated by the Social Interventions Research and Evaluation Network (SIREN) from the University of California San Francisco. The Child Savings Account Program will be assessed by Drs. Adam Schickedanz and Monique Holguin, co-directors of the University of California Los Angeles Medical-Financial Partnership.
About Covered California
Covered California is the state’s health insurance marketplace, where Californians can find affordable, high-quality insurance from top insurance companies. Covered California is the only place where individuals who qualify can get financial assistance on a sliding scale to reduce premium costs. Consumers can then compare health insurance plans and choose the plan that works best for their health needs and budget. Depending on their income, some consumers may qualify for the low-cost or no-cost Medi-Cal program.
Covered California is an independent part of the state government whose job is to make the health insurance marketplace work for California’s consumers. It is overseen by a five-member board appointed by the governor and the Legislature. For more information about Covered California, please visit www.CoveredCA.com.

